How AI Automation Improves Healthcare Revenue Cycle Management
- Ali Hasan
Contents
Real-Time Eligibility Verification in Revenue Cycle Management:
Healthcare revenue cycle management faces escalating challenges such as rising claim denials, fragmented billing processes, and administrative bottlenecks that slow reimbursements and increase costs. AI automation is no longer just a buzzword—it’s becoming a critical tool to enhance accuracy and speed across revenue cycles.
Research by McKinsey shows that AI-driven solutions can reduce denial rates by up to 70%, dramatically improving financial outcomes. As healthcare providers explore automation, integrating AI into key operational areas—like hospital resource allocation—helps ensure resources are aligned with patient needs and billing requirements. Similarly, leveraging AI in healthcare logistics automation optimizes workflow efficiency across care delivery and billing.
Kodexo Labs specializes in AI development services tailored for healthcare, helping organizations adopt intelligent automation that supports cleaner claims and smoother reimbursements without disrupting clinical workflows.
Understanding the Revenue Cycle in Healthcare:
What Is Revenue Cycle Management (RCM)?
To understand what revenue cycle management is, think of it as the financial nervous system of any healthcare organization. From the moment a patient schedules an appointment to the time the final payment is posted, the revenue cycle management process ensures care is translated into revenue — accurately, compliantly, and efficiently.
Here’s how the medical revenue cycle management system works, stage by stage:
Traditionally, these steps rely on manual inputs and siloed systems — leading to data errors, missed payments, and slow cash flow. But that’s rapidly changing.
AI-powered platforms are now embedded at each layer of the revenue cycle to improve speed and reduce error rates. At Kodexo Labs, we implement healthcare software development solutions that use artificial intelligence to automate:
- Insurance verification at the scheduling stage
- Data validation and duplicate detection during registration
- NLP-enhanced accuracy in medical coding
- Smart invoice auditing in billing workflows
- Real-time rule checks during claim submission
- Automated matching and alerting in reimbursement and appeals
This is not just automation — it’s augmentation.
With AI woven into the revenue management cycle, healthcare organizations reduce denied claims, accelerate reimbursement timelines, and gain end-to-end visibility into performance. More importantly, they shift from firefighting operational bottlenecks to running a scalable, intelligent, and compliant billing operation.
That’s why revenue cycle management in healthcare today is as much a data challenge as it is a financial one — and AI is the tool making it solvable.
Stay Updated—Join Our Newsletter!
Newsletter
Persistent Challenges in Traditional RCM:
Despite its importance, the revenue cycle management process in healthcare still struggles under layers of operational inefficiencies. Manual processes and disconnected systems create bottlenecks that cost providers time, money, and patient trust.
Here are five persistent revenue cycle management healthcare challenges faced by modern practices:
1- High Claim Denial Rates:
Denials have increased by more than 23% between 2016 and 2022, often due to data mismatches, missing authorizations, and outdated payer rules (Becker’s Hospital Review).
2- Human Data Entry Errors:
3- Fragmented Systems:
4- Delayed Reimbursements:
5- Manual Appeals Process:
These issues are more than just operational friction. They represent lost revenue, increased burnout, and diminished scalability — especially in hospital revenue cycle management environments with complex, high-volume workflows.
At Kodexo Labs, we tackle these challenges through enterprise-grade software development services that integrate AI, automation, and analytics directly into the revenue cycle — helping providers replace manual bottlenecks with intelligent workflows.
It’s not just about doing RCM faster. It’s about doing it right — with systems that adapt, learn, and scale.
Read More Related Blogs:
How AI Automates Healthcare Revenue Cycle Management:
Core Technologies Enabling AI in Automated Revenue Cycle Management:
The foundation of AI in revenue cycle management lies in the synergy of three core technologies: predictive analytics, machine learning, and natural language processing (NLP). At Kodexo Labs, we don’t use these as buzzwords — we build them into custom RCM systems that solve the operational gaps virtual healthcare assistants face every day.
Let’s break down how each technology transforms revenue workflows:
Predictive analytics enables healthcare organizations to move from reactive to proactive financial operations. By analyzing historical claims data, payer behavior, and patient demographics, AI models can forecast denial risks, reimbursement delays, and claim approval likelihood.
For example, Kodexo Labs integrates predictive scoring into real-time eligibility workflows. This allows front-desk systems to flag high-risk coverage issues before the patient is even seen — giving staff time to correct errors or obtain prior authorizations.
These data-driven insights form the basis for smart interventions, helping practices reduce denials and optimize resource allocation across the entire revenue cycle.
Machine learning in revenue cycle management powers continuous system improvement. Rather than rely on hard-coded rules, ML algorithms learn from claims history, payer feedback, and process outcomes — allowing them to automatically refine scrubber rules, flag anomalies, and adjust billing logic.
Kodexo Labs trains ML models to handle:
- Claim classification
- Error detection
- Underpayment prediction
- Workflow triage
These systems continuously learn from payer patterns and reimbursement data, improving with every billing cycle. That’s the core of how machine learning in revenue cycle management replaces static rule-based engines with dynamic, data-trained workflows.
At Kodexo Labs, our approach is grounded in real-world healthcare applications. We apply the core principles of what machine learning is to build solutions that automate billing, predict denials, and optimize claim success — all without disrupting your existing infrastructure.
Natural language processing in healthcare enables systems to read and understand unstructured text — like physician notes, discharge summaries, and lab reports — with accuracy and speed.
Kodexo Labs integrates NLP models into the documentation and coding process to:
- Extract diagnoses and procedures
- Map them to standardized codes (CPT/ICD/HCPCS)
- Flag clinical contradictions or missing context
- Populate claims with validated language
This reduces manual coding effort, increases claim accuracy, and ensures compliance — especially in specialties with complex narratives like oncology or cardiology.
Together, these AI technologies form a modular architecture that elevates revenue cycle management from a passive workflow to a responsive, intelligent system.
At Kodexo Labs, we design these systems not as standalone tools, but as interoperable engines inside your RCM stack — working behind the scenes to ensure accuracy, speed, and financial sustainability.
Real-Time Eligibility That Doesn’t Rely on Portals or PDFs
Let's Talk
How Kodexo Labs Automates the Entire Revenue Cycle:
At Kodexo Labs, we don’t offer one-size-fits-all billing tools. Instead, we engineer custom AI automation pipelines designed to integrate directly into your existing RCM stack — streamlining key functions like claim scrubbing, payment reconciliation, denial management, and patient communication.
Here’s how we optimize each phase of the revenue cycle using purpose-built AI.
Submitting clean claims is one of the biggest cost-savers in the entire revenue cycle. Kodexo Labs builds AI-driven scrubbing logic that proactively catches errors before submission — reducing rejections and saving hours of administrative rework.
These AI workflows are designed to:
- Apply payer-specific validation rules based on live contract logic and historical denial data
- Combine standard edits (e.g., NPI mismatches, missing fields) with custom business rules defined per organization
- Trigger real-time edit checks that flag ICD/CPT mismatches, authorization issues, and formatting violations
This reduces the chance of downstream claim denials while accelerating approvals and reimbursements.
By embedding these systems into our clients’ automated medical billing software, we enable repeatable, high-accuracy claim scrubbing AI workflows tailored to each payer relationship — not generic tools.
Once claims are submitted, the payment process is often where revenue leakage occurs.
Kodexo Labs implements automated payment reconciliation systems that help providers match, validate, and analyze reimbursements against contracts.
Our machine learning-based workflows handle:
- ERA Parsing — standardizing and reading remittance data across payers
- 24/7 Payment Matching — linking payments to services rendered, even in high-volume environments
- Underpayment Flagging — surfacing discrepancies between contract rates and received amounts
- Contract-Based Validation — ensuring each transaction aligns with negotiated terms
These systems form the backbone of scalable, audit-ready medical billing reconciliation software — enabling complete control over healthcare RCM payments without spreadsheet chaos.
Denied claims stall cash flow and require hours of follow-up — but many denials are preventable with the right data strategy.
At Kodexo Labs, we use machine learning models trained on historic payer behavior and rejection patterns to automate:
- Denial detection — identifying root causes based on trends in submission errors or payer responses
- Appeal generation — drafting tailored appeal letters using payer-specific guidelines
- Submission routing — directing appeals through the appropriate fax, mail, or portal channel
Traditional denial management often forces billing teams into reactive cycles—fixing errors only after reimbursements are delayed. Kodexo Labs shifts this paradigm by applying AI earlier in the workflow, where it can actually prevent denials from occurring in the first place.
By learning from historical payer responses and rejection codes, our AI surfaces denial-prone patterns—before submission. This enables teams to proactively correct issues, auto-generate payer-compliant appeals, and route them through preferred channels without manual formatting or repeated data entry. The result? Faster resolutions, fewer downstream bottlenecks, and a noticeable reduction in time spent chasing preventable errors.
Revenue cycle automation doesn’t end with payers — it extends to how patients understand, trust, and pay for their care.
Kodexo Labs develops smart communication systems that improve billing clarity and responsiveness by automating:
- Real-time cost estimation — showing patients what they owe before care is delivered
- Balance transparency — syncing insurance coverage with service-level billing details
- Automated follow-ups — sending reminders and payment links at the right time, through the right channel
At the heart of this is our integration with tools like AI scribe — which supports real-time coverage validation and accurate documentation, removing the usual billing confusion patients face.
All of this is built using our custom product development services, giving providers modular control and future-ready patient experience infrastructure.
Top Benefits of AI in Medical Billing: Faster Claims & Fewer Denials
1- Faster and More Accurate Claims:
In the fast-paced world of healthcare billing, speed and accuracy are paramount. AI-powered tools like eligibility verification AI and advanced claim scrubbers help providers submit clean claims rapidly, reducing delays caused by incorrect or incomplete data.
Kodexo Labs implements AI claim validation systems that perform real-time eligibility checks and multi-layered claim scrubbing. These systems detect errors before submission, ensuring claims are formatted correctly and compliant with payer-specific rules.
The result? Practices experience up to 30% faster medical billing reimbursement cycles, supported by industry data from sources such as McKinsey & Company.
2- Reduced Denials and Financial Leakage:
Denials and financial leakage represent major revenue drains for healthcare providers. Kodexo Labs leverages AI-powered denial trend detection and AI denial prediction to minimize these costly issues.
By analyzing historical claim data and payer patterns, our AI identifies systemic denial causes early, allowing for automated interventions that prevent errors from recurring. When denials do occur, our systems automate appeal generation and submission workflows, accelerating resolution.
This approach substantially reduces healthcare financial leakage by identifying denial patterns and automating corrective workflows, resulting in significant reductions in denial rates and faster revenue recovery.
To build accurate AI models that detect these patterns effectively, Kodexo Labs relies on expert data annotation specialists who meticulously label healthcare datasets—an essential step in training reliable predictive algorithms.
3- Cost Savings and Labor Efficiency:
AI’s impact extends beyond revenue — it drives operational savings and workforce productivity:
- Reduces manual workload by automating repetitive data entry, claim reviews, and document processing
- Automates repetitive administrative tasks such as patient follow-ups, billing inquiries, and report generation
- Enables staff to focus on care coordination, compliance oversight, and complex exception handling
These efficiencies translate into meaningful labor cost savings healthcare organizations can reinvest into patient care and innovation.
Cut Denials Before They Happen With AI-First RCM Workflows
Let's Talk
Real-World Impact: Kodexo Labs’ Smart Medical History Revolutionizes Patient Intake
The Challenge: Complex, Time-Consuming Patient Intake Processes
Additional challenges includes:
- Variations in speech patterns and accents complicating medical terminology recognition
- Resistance to new technology adoption within regulated environments
- The need to accommodate diverse healthcare organizations—from solo practitioners to large networks
- Ensuring compliance with region-specific licensing and data security regulations
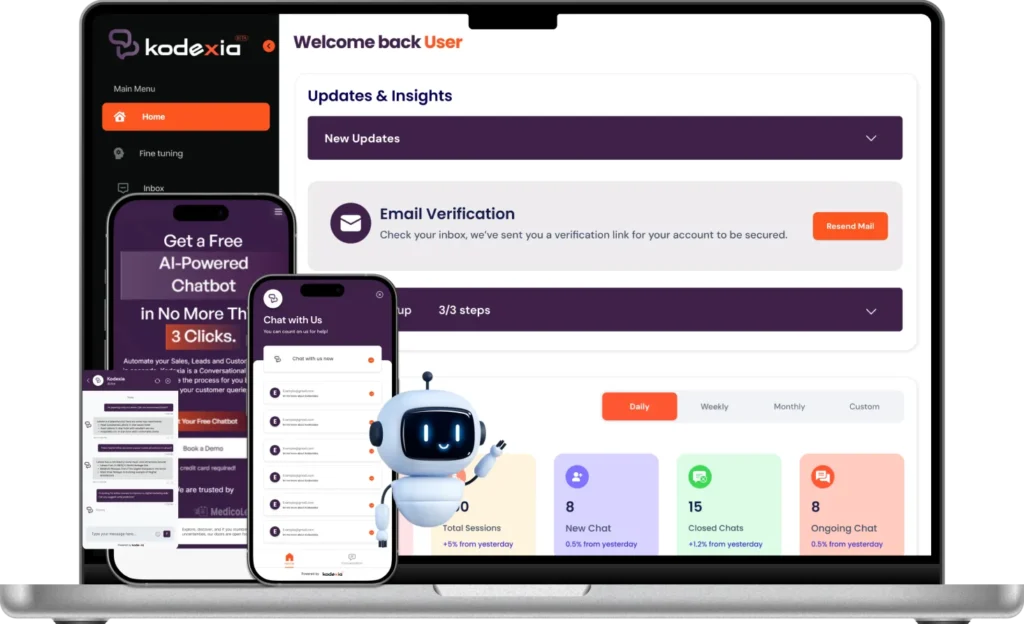
The Solution: Smart Medical History — AI-Powered, Voice and Text-Based Medical Interviewing
Kodexo Labs developed Smart Medical History (SmartMedHx), an intelligent platform designed to automate and simplify the medical intake process. By integrating advanced voice recognition and natural language processing, the platform collects examinee information accurately and efficiently, generating real-time, dynamic reports that seamlessly fit into existing workflows.
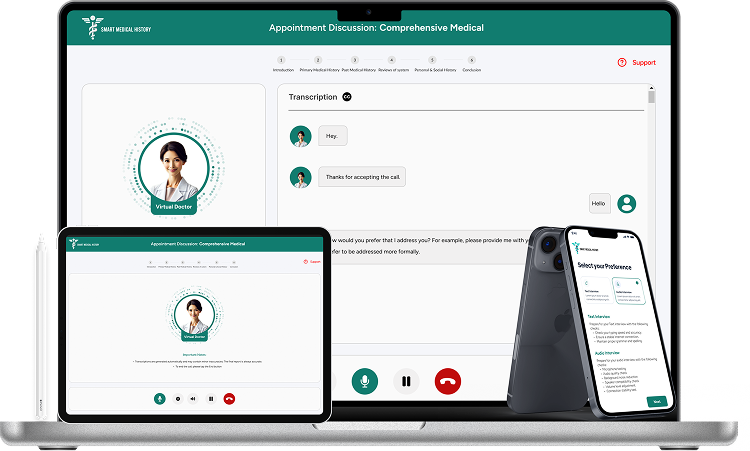
Key Features Include:
1- Multi-Modal Interview Flows:
2- Voice-Enabled Experience:
Patients can speak naturally, improving engagement and reducing friction.
3- Intelligent Provider Assignment:
4- Timezone-Smart Scheduling:
5- Robust Security:
Overcoming Technical and Market Challenges:
- Developed accurate medical terminology recognition despite accent and speech variation
- Built an intuitive UI that integrates smoothly into daily provider workflows
- Engineered smart session management to handle disconnections and idle time without data loss
- Addressed licensing and compliance friction through customizable agreements and configurations
The Impact: Measurable Improvements in Efficiency, Accuracy, and Patient Experience
- Up to 40% reduction in patient intake time through automation, easing administrative burdens.
- Stronger data confidence with real-time validation and adaptive questioning, reducing rework and errors
- Scalable across practice sizes, from solo practitioners to multi-location networks, with minimal setup.
- Enhanced patient comfort via conversational, human-like interactions, improving completeness and accuracy of data.
- Actionable clinical insights delivered instantly through dynamic, filterable reports.
By automating and enhancing the intake process, Smart Medical History improves clinical workflows and supports a more efficient and accurate revenue cycle—critical to timely and accurate billing and reimbursement.
This case exemplifies how Kodexo Labs blends cutting-edge AI with healthcare domain expertise to solve real-world challenges and improve financial and operational outcomes.
Overcoming Barriers to AI Adoption in Revenue Cycle Management:
The Real Barriers Holding Back Transformation:
Adopting AI in healthcare revenue cycle management (RCM) isn’t without its hurdles. Many organizations face structural, cultural, and technical challenges that slow down or block effective implementation.
Kodexo Labs understands these barriers to healthcare AI adoption deeply and offers tailored strategies to overcome them.
1. Operational Inertia and Cultural Resistance:
Healthcare organizations often struggle with change fatigue and resistance from teams accustomed to manual workflows. Staff may fear job loss or loss of control.
Kodexo Labs mitigates this through comprehensive onboarding and change management programs that emphasize AI as an augmentation tool, not a replacement. Customizable rule-based AI solutions help teams retain control while automating low-value tasks, easing cultural resistance.
2. Fragmented Data and Technology Ecosystems:
Disconnected systems across scheduling, EHR, billing, and payer platforms make seamless AI integration difficult.
Kodexo Labs tackles this challenge by architecting solutions that support bi-directional integration and centralized dashboards, unifying fragmented data sources. This approach improves real-time visibility and operational coherence without requiring rip-and-replace system overhauls.
3. Limited In-House Technical Expertise:
Many healthcare practices lack the AI and data science expertise necessary for implementation and maintenance.
Kodexo Labs offers white-glove onboarding, training, and support with dedicated success managers, ensuring clients don’t need deep technical know-how to operate sophisticated AI tools. Our AI consulting services provide expert guidance every step of the way.
4. Uncertainty Around ROI and Timeline:
Providers often hesitate because they’re unsure about how quickly AI will deliver measurable benefits or if the investment is worthwhile.
Kodexo Labs addresses this by implementing phased rollouts and clear KPIs aligned with client goals. Our proven development process enables AI systems to go live within weeks, with clients typically reporting significant reductions in manual workload and faster reimbursements within the first quarter.
5. Fear of Losing Human Oversight:
Some organizations worry that AI adoption will reduce human control, leading to errors or regulatory risks.
Kodexo Labs designs AI workflows to augment human decision-making, not replace it. Clients receive ongoing performance insights through dedicated success managers and billing professionals, ensuring transparency and oversight remain central throughout automation.
Kodexo’s Strategic Approach:
Kodexo Labs takes a methodical and client-centered approach to implementing AI-driven automation in healthcare revenue cycle management. Our goal is to deliver custom AI revenue cycle management solutions that seamlessly integrate with existing workflows and drive measurable improvements.
Here’s how we do it:
1. AI Audit:
Our process begins with a detailed AI audit to evaluate your current revenue cycle operations, identifying inefficiencies and pinpointing where AI can generate the highest impact. This foundational step is part of our expert software consulting approach, ensuring that automation aligns precisely with your needs.
2. Workflow Mapping:
3. Data Integration:
Seamless data integration across electronic health records, billing platforms, and payer systems is critical. Kodexo Labs connects these disparate sources to create a unified data pipeline, ensuring your AI models are fueled by consistent, high-quality information. This integration is a key pillar of our AI integration services, providing a reliable backbone for automation.
4. Success Manager Support:
5. Continuous Monitoring:
Stay Updated—Join Our Newsletter!
Newsletter
What the Future Holds for AI in Healthcare RCM:
1. Emerging Trends:
The landscape of generative AI in healthcare billing is rapidly evolving, promising to revolutionize how providers manage contracts, communicate with payers, and maintain compliance.
Advanced generative AI models are increasingly applied to payer contract analysis, enabling automated parsing of complex, jargon-heavy agreements. This accelerates the identification of key payment terms, rates, and obligations, reducing manual review times and minimizing costly errors.
Google’s Med-PaLM and other cutting-edge research highlight the transformative potential of generative AI to simplify and automate these traditionally labor-intensive tasks (Google Med-PaLM).
LLMs for medical billing are reshaping payer-provider interactions by automating message drafting, claim inquiries, and real-time negotiation support. These models understand complex medical and billing terminology, enabling more precise and efficient communications.
HIMSS research indicates that integrating LLMs can reduce response times and improve accuracy in dispute resolution processes, ultimately speeding reimbursements and improving cash flow.
Regulatory compliance remains a critical challenge in healthcare RCM. AI-driven compliance automation tools monitor claims for adherence to evolving payer rules, detect anomalies, and generate audit-ready reports.
These AI systems continuously learn from policy updates and payer feedback, ensuring that organizations stay ahead of regulatory changes with minimal manual oversight.
Kodexo Labs actively integrates these emerging AI capabilities into our solutions, preparing healthcare providers to thrive in an increasingly complex and AI-driven environment.
For a deeper dive into how generative AI is shaping healthcare, explore our detailed guide on the future of generative AI in healthcare.
Read More Related Blogs:
Preparing for Next-Gen RCM:
Healthcare organizations preparing for future-ready revenue cycle management should consider these key steps:
- Run an AI audit to evaluate existing workflows and pinpoint areas where AI can add value.
- Identify automation-ready processes, focusing on repetitive or manual tasks ripe for AI enhancement.
- Deploy pilot workflows to validate AI solutions on a small scale before full implementation.
- Partner with experienced teams to ensure smooth and scalable AI deployment medical workflows aligned with organizational needs.
Free Up 30% of Admin Time by Automating What Doesn’t Need Humans
Let's Talk
Conclusion and Next Steps:
AI-driven advancements in revenue cycle management are reshaping healthcare billing by streamlining workflows, reducing claim denials, and improving financial transparency. These innovations enhance operational efficiency and help healthcare organizations reclaim revenue that was previously lost to manual errors and fragmented processes.
Adopting effective revenue cycle automation solutions enables healthcare providers to optimize their billing systems while maintaining compliance and improving patient experience. Preparing for this transition involves assessing current capabilities, identifying automation opportunities, and carefully deploying scalable AI tools that fit within existing workflows.
For organizations seeking to understand their AI readiness and explore practical next steps, tools like audit checklists can provide valuable insights. Engaging with experts knowledgeable in healthcare AI integration can support a smoother, more effective adoption of next-gen revenue cycle tools.

Author Bio
Read More Blogs
Know What Causal AI Is, How It Works and Why It Is Important?

The Future of Business Automation Starts with AI Agents